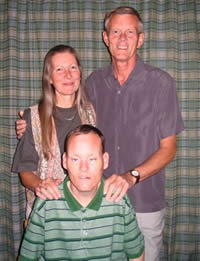
Stephanie Stollery’s Story
Terry Stollery first started to feel ill in the autumn of 2005.
One day he said: “Oh, I think I need to go to the doctor’s”.His wife Stephanie got on the phone straight away. It was not like Terry to complain. He was a strong, quietly dignified man.
She said: “In hindsight I think there were tell-tale signs before, but Terry just got on with things, that is how he was.”
At first it was put down to constipation and he was given some tablets, but he struggled and was later referred to Ipswich Hospital.There he had an endoscopy in January 2006 and a scan in the same month.
In the meantime, on January 23rd, while they were waiting for the scan results to come back, Terry, a well-known painter and decorator, collapsed at work, and was taken to the hospital. They operated on a perforated bowel on January 24th. During surgery doctors found a tumour on the outside of his colon which they said had been there for between ten and 12 years.
Stephanie, 54, recalled: “He was offered chemotherapy and radiotherapy and he took it all in his stride. He was so determined to get out of the hospital as soon as possible. He did not want to be waited on. He said the illness was like having flu but a bit stronger. He was just very positive.”
It was August 2008 when doctors at Ipswich Hospital confirmed the tumour had returned and the only way to try and beat it was aggressive chemotherapy. Terry said at the time: “Do whatever you have to do.” But the chemotherapy made him feel too ill, he couldn’t keep his food down and the doctors said it was killing him quicker than the disease. So Terry decided he would fight it on his own – through sheer determination and spirit.”
It was then that Terry was discharged from hospital care and his care was handed over to St Elizabeth Hospice, GPs and district nurses.
“That day he went home and put a red dot on the calendar. He said it was his second birthday.” It was a symbol of him being positive about his illness and vowing to fight it and carry on with life.
“I don’t think Terry wanted to go to the hospice at first. Being a man I didn’t know how he would react when he was offered day care services. It all sounded really good and useful but I just wasn’t sure it was for him. He said he would go to day care once, but from the first day I think he felt he could benefit as well as put something back in.”
Their first assessment was with the hospice’s medical director Dr Kelvin Bengtson.
Stephanie said: “He was just so lovely. He spoke to us in such a way that covered absolutely everything that we had had questions about. It was after that Terry surprised me and said he would give day care a go and he went there each week for six weeks.
“It was good to have people around you that knew you and if you were worried about something you could ask them any little thing.
“He was always coming home with things he had bought or made there and was always thinking of ideas that he and the other patients could do as a group.”
At the hospice Stephanie was offered family support services including complementary therapy. Both Stephanie and Terry benefited from hand massages.
After six weeks of day care sessions, Terry returned to the hospice to the nurse-led clinic for blood transfusions in the comfortable out-patient’s room. He returned to day care when he could.
“That was lovely, rather than him having to go back to the hospital, it was more relaxed, ” remembered Stephanie.
Sometimes when Terry needed symptom control at home he was visited by Hospice at Home, a reactive nurse-led team.
The Hospice’s occupational therapist also played a part in the many services Terry and his family were able to call upon.
Music therapy was also offered to the family and this played a crucial part in their journey and their son Steven, who has special needs, benefited from it.
As Terry neared the final stages Stephanie stayed with him at the Hospice. She would play the CD of Steven’s music therapy session and that was a great comfort to them. Steven also visited his dad at the Hospice again and they spent time together in the family room. Steven could now see how his dad had deteriorated.
“Steven found this hard, he could see Terry could not communicate and brought the reality of the situation home.
Stephanie said: “The nurses were wonderful, they knew when to step back and when to be there. They were always available when we needed them. One night they put a bed down for me at 2.30am and we thought three times that Terry had gone. But it wasn’t until around 24 hours later. The nurse said his breathing had changed and she thought I would like to be with him, and that was lovely. He seemed at peace. It was the first time he was free of pain.
“Afterwards there was no rush I was allowed to stay with Terry as long as I needed to.”
Terry died on April 21st 2009 aged 61.
Stephanie said Terry was also a very private man and always supportive of others.
When Stephanie saw Steven next he gave her a big hug and burst into tears. “He has been remarkable. He had music therapy the following week and came back to the Hospice for it and was fine. He chose his own flowers for the funeral and was very adult about that. At the funeral someone said he was like a ‘normal’ son, giving me support. He was so strong.”
“The hospice is a wonderful place. From the very first assessment appointment, through day care and as an in-patient, the Hospice guided us through Terry’s illness.
“When we knew we couldn’t change what was going to happen, we tried to take all the positives from the situation and work with it. This was made much easier with all the support from every person connected with the Hospice along with our family doctor and staff at the surgery such as district nurses and receptionists.
“The support that is given, not just for the person that is ill but the whole family, is wonderful. Terry chose to be there. It was so relaxed. The staff and volunteers were lovely. The nurses are always there when you need them. It is also a happy place. We did have a laugh on the ward. It was good having that support and knowing it is just not about having the medical care. It was everything else which made it so much easier. It’s not just a place where you go to die. It’s about quality of life.
“I have visited the hospice several times since and am always made very welcome. The support doesn’t stop when the person dies.
“We knew we could not change the inevitable, you work with it, with the support of all the people around you. Terry was so positive because of that support. I think that is why I am so positive now.”



